It has long been thought that the constant pounding of running can cause degeneration of the lumbar disc, however this theory has recently been debunked. A 2017 study from Deakin University in Victoria has found that people who regularly run or walk have stronger and healthier discs in their spine compared to people who do not exercise.
It was shown that through running or brisk walking, the disc showed improved hydration, increased protein content and growth of the disc. The control group for the study were sedentary, non-active adults – whom showed no change in disc characteristics.
One important factor from this study is that the brisk walking and running groups both showed the same amount of improvement in disc health. So, you don’t have to be a runner to improve the health of your discs, walking is fine as well!
The authors concluded that the response of the disc to running is very similar to the response of muscle in resistance training.
What if I have a disc injury?
If you have a disc injury, movement is good for it! It allows the disc to recover through getting nutrition to the disc to allow for repair. If minimal movement occurs at the disc, healing will be therefore very slow.
Why is this so?
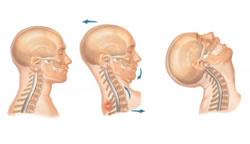
Discs get their nutrition through diffusion from the bony endplate of the vertebra above and below. The way this diffusion works is through movement. The constant loading and unloading of the spine through walking or running allows for the flow of nutrients to the disc. In sedentary individuals, the diffusion of nutrients is poor due to the lack of movement, hence why degeneration and dehydration of the discs is more likely.
So the take home message is to move more to strengthen and improve your back health. It also doesn’t have to be intense running, a brisk walk is also as beneficial. Walking with a disc injury is also an important part of the recovery, as it allows for the disc to receive nutrients to allow for repair to occur.
Belavy, D. L. et al. Running exercise strenghtens the intervertebral disc. Sci. Rep. 7, 45975; doi:10.1038/srep45975 (2017)
Mitchell Roberts – Chiropractor