I often have patients presenting to me complaining of repetitive pain-free joint clicking (crepitus) of their knee or shoulder. This can often cause anxiety as they associate this clicking with arthritis and joint degeneration. It tends to be more common in the morning and after a period of inactivity, though reduces with movement / once warmed up.
A 2017 study by Robertson et al found that knee crepitus lead to worry, anxiety and eventually fear-avoidance behaviour – meaning they stopped doing their regular exercise because of the sounds.
Thankfully, joint crepitus is entirely normal. A 1987 study by McCoy et al found that of 250 normal knees studied (no prior injury and pain free), 99% had knee crepitus!
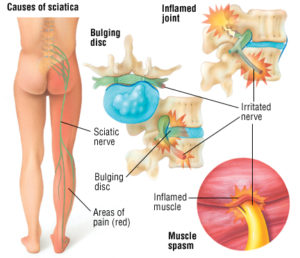
So what is causing the noise? First off, it is not bone on bone – as this would be very painful and uncomfortable. The noise is fluid moving within the joint and/or tendons/ligaments rubbing and flicking against the bone on the outside.
The role of health practitioners should be to educate patients and eradicate their fear that no damage is being caused by the sounds.
Knee Crepitus = Normal
The concluding message is that clicking and creaking in joints is very common and is not a sign of joint damage – as long as there is no associated pain or swelling. If you do have any concern, come in and see us at Mona Vale Chiropractic Centre for a thorough assessment.
McCoy G, McCrea JD, Beverland D, Kernohan G, Mollan RB. Vibration arthrography as a diagnostic aid in diseases of the knee. J Bone Joint Surgery (Br) 1987; 69-B, 2: 288-293
Robertson CJ, Hurley M, Jones F. People’s beliefs about the meaning of crepitus in patellofemoral pain and the impact of these beliefs on their behaviour: A qualitative study.Musculoskelet Science and Practice. 2017 Apr;28:59-64
Mitchell Roberts – Chiropractor